by Anne Montgomery, PhD, Mercer University School of Medicine Rural Health Sciences PhD Program Director and GRHIC Biostatistician
Exploring Rural Perspectives on Whole-Body Donation for Research in Georgia
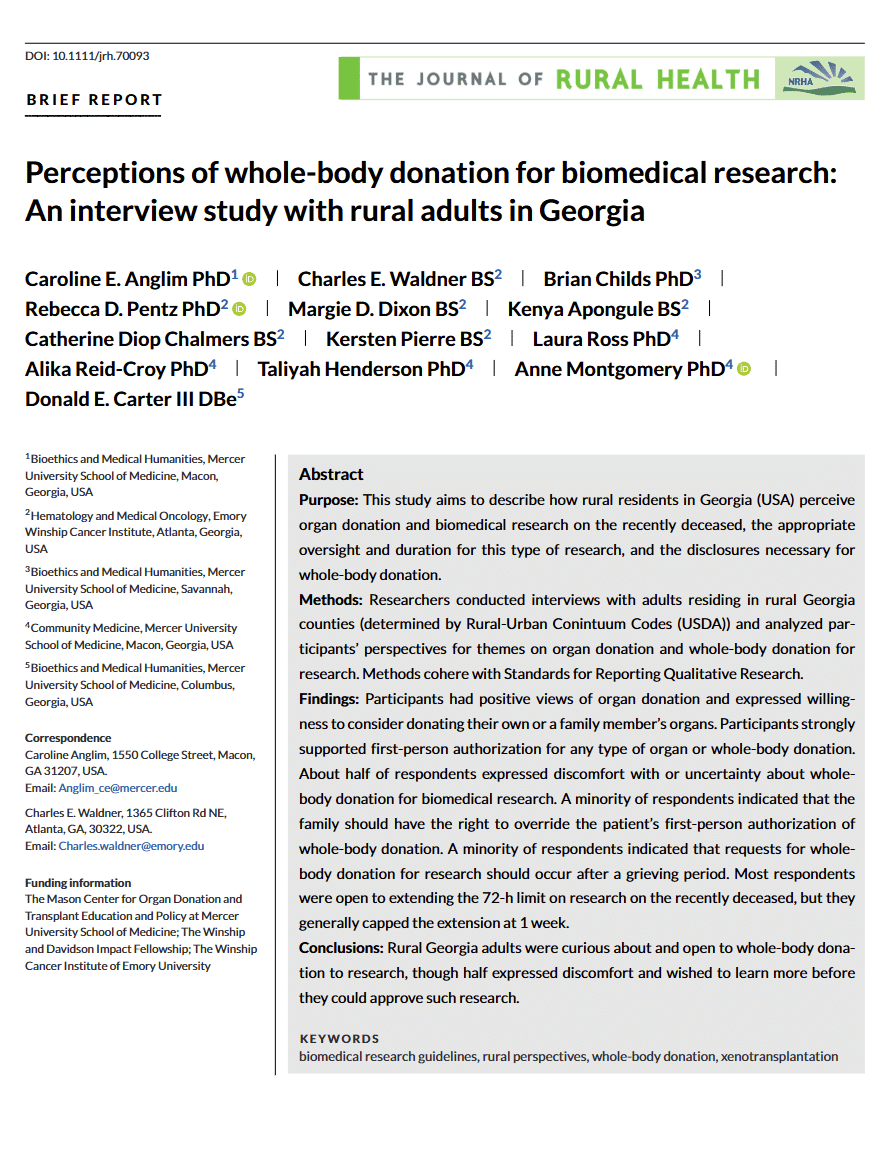
The Mercer University School of Medicine Rural Health Sciences PhD team at the Georgia Rural Health Innovation Center (GRHIC) contributed to a study published in The Journal of Rural Health. In the study, the team examines how adults in rural Georgia view organ donation and whole-body donation for biomedical research. This research highlights critical insights into a topic often overlooked in rural communities and sheds light on public attitudes toward postmortem research.
Team Effort from Inception to Publication
This article is the result of a collaborative effort led by Caroline Anglim, PhD, and her team of the Bioethics Department at the School of Medicine. The team at the Georgia Rural Health Innovation Center included School of Medicine associate professor Anne Montgomery, PhD, with three former School of Medicine PhD students and GRHIC research assistants: Taliyah Henderson, PhD, Alika Croy, PhD, and Laura Ross, PhD.
Understanding Rural Perspectives
Much of the existing research on organ and whole-body donation has focused on urban or academic populations, leaving rural perspectives underexplored. The study aimed to fill this gap by interviewing adults across rural Georgia counties. Participants were recruited from local primary care clinics, community networks, and GRHIC’s newsletter. Eligible participants were adults living in rural counties.
Using semi-structured interviews, the team spoke with 19 participants representing a range of ages, education levels, and income backgrounds. Most participants expressed general support for organ donation. Many indicated that they were registered donors or willing to authorize donation for family members. Whole-body donation for biomedical research, however, elicited more nuanced and ambivalent responses. About half of participants were open to donating their body for research, while the remainder expressed discomfort, conditional support, or refusal.
Key Findings
Several themes emerged from the study’s analysis:
- Support for First-Person Authorization: Most participants stressed that individuals should have the main authority to decide whether their body is donated for research. Only a small minority felt families should be able to override these wishes, and even then, opinions varied on the extent of family authority.
- Moral and Spiritual Considerations: Nearly half of respondents expressed uncertainty or discomfort about whole-body donation after brain death, particularly when a heartbeat or circulation continued. These concerns reflected moral questions about the boundary between life and death.
- Communication and Timing: Participants highlighted the importance of respectful and clear communication when requesting donation. Some preferred requests occur after death, while very few supported approaching individuals before death.
- Research Duration: The study also explored attitudes toward the existing 72-hour limit on postmortem research. Most participants were open to modest extensions, typically up to one week, recognizing the potential benefits for biomedical research while maintaining ethical safeguards.
Implications for Practice and Policy
These findings suggest that rural populations are generally curious about and willing to support whole-body donation for research, provided their autonomy is respected and ethical practices are followed. The study underscores the need for thoughtful engagement with rural communities, clear communication, and culturally sensitive approaches when discussing postmortem donation.
The insights are particularly relevant for emerging biomedical research, such as research into xenotransplantation (i.e., the use of animal organs to replace human organs). Ethical access to recently deceased human bodies can advance scientific knowledge significantly.
This publication represents a crucial step in understanding rural perspectives on biomedical research and organ donation. Findings can inform healthcare providers, research institutions, and policymakers in designing ethical and community-aligned practices that respect first-person authorization while considering family roles.
Special thanks to Dr. Henderson, Dr. Croy, and Dr. Ross for their foundational contributions, as well as to the rural Georgians who participated in this study. Their voices are central to ensuring research practices align with community values and ethical standards. Special thanks to community partners, regional health systems, and the many county leaders who generously shared data, time, and insights during this process.
Read the Article
Access the full article in The Journal of Rural Health https://onlinelibrary.wiley.com/doi/full/10.1111/jrh.70093. Feel free to reach out to Montgomery_a@mercer.edu to receive a PDF version of this article.
Colleagues, community leaders, and policymakers are encouraged to explore these findings and consider their implications for ethical biomedical research in rural communities.
