By Amanda A. Livingston, Director of Communications and Events
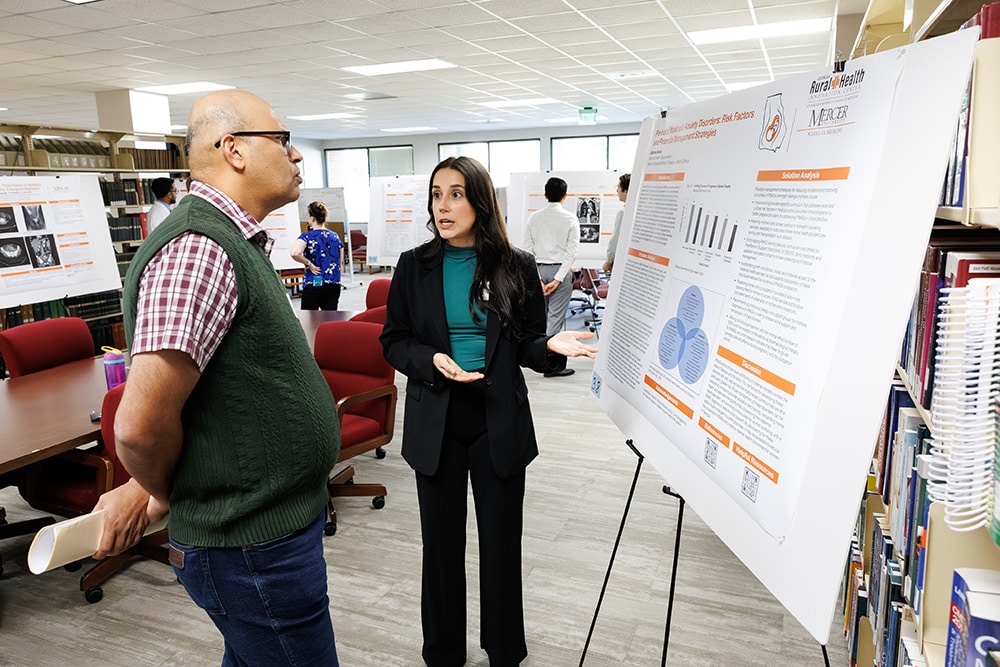
Sydnee Burke, a graduate of the Georgia Rural Health Innovation Center’s Maternal Health Observership and second-year medical student, presented her research poster, titled “Perinatal Mood and Anxiety Disorders: Risk Factors and Potential Management Strategies,” at Mercer University School of Medicine’s Joint Research Conference. The conference unites faculty and students from the School of Medicine’s three campuses and the School of Pharmacy for an interprofessional symposium showcasing the latest advancements in Mercer’s health-related research. Burke tied for top recognition on the Macon campus in the epidemiology category.
Burke’s research project, a requirement of the summer Maternal Health Observership Program, was inspired by the Maternal Health Symposium, hosted by the Georgia Rural Health Innovation Center (GRHIC) in June. It was during this event where she learned that mental health conditions, including perinatal mood and anxiety disorders, are the second leading cause of death for pregnant women in Georgia. This alarming statistic motivated her to explore how to improve outcomes for women suffering from these conditions in rural communities.
Burke’s research took the form of a problem analysis and solution proposal, relying on an extensive literature review. She identified two major challenges: the lack of proper screening for maternal mental health issues and insufficient provider education on treatment pathways. A solution she proposed is to include more education on maternal mental health in medical school and health care professional programs that focus on not just screenings but also on how to recognize disorders and what treatment options are suitable. She said, “There are a lot of things that we can implement into clinical practice to help improve outcomes.”
Burke credits much of her inspiration to mentors such as Keisha Callins, MD, MPH, who served as a preceptor for the observership program. “Every time she had a woman come in, she always asked her ‘How are you feeling? How’s mental health going.’ She was always doing those check-ins, which is something that I think is really important, that everyone as a provider could be doing to further reduce incidences of perinatal mood and anxiety disorders,” said Burke.
Though she has particular interest in women’s health care, Burke is leaning toward family medicine. “I really like the variety of being able to do some OB-GYN in my practice, but then also be able to treat everyone,” she said. “I’ve talked about that with Dr. Callins, and she always says, ‘You know, just because you’re not practicing OB-GYN doesn’t mean you’re not practicing women’s health care.” Burke looks forward to serving women, their children and spouses.
As a School of Medicine Nathan Deal Scholar, Burke is committed to practicing in a rural setting after residency. She envisions a future where she not only treats patients but also advocates for community-wide improvements, using population health data to address specific challenges. “I think something that I really want to do when I’m a physician one day is not only just focus on my patients and my practice, but really be involved in the community so that I can gain a better understanding of what people are struggling with,” she said.
While shadowing rural physicians, Burke gained meaningful understanding of the unique challenges they face and the strong connections they build with their patients. One memorable moment involved a patient of Justin Peterson, MD, a practicing rural OB-GYN physician in Douglas, and an observership preceptor. The patient prepared homemade empanadas for his lunch—a gesture that underscored the deep bonds of trust in rural medical practice. “I think that’s something really special, and I’m very glad that the Maternal Health Observership allowed me to see,” Burke said.
Burke’s participation in the Maternal Health Observership left a lasting impression. “I would really like to give a huge thank you to GRHIC and the Maternal health Observership. It was a really great experience,” she said. “It gave me so much valuable time to not only work with OB-GYNs, but work with rural physicians and gain better insight into the problems that they face day-to-day that you wouldn’t see if you were a physician working in Atlanta.”
